The child’s fever is accompanied by these symptoms, and it must not be treated as a cold.
Original PerrineWANG medical pediatric channel
For medical professionals’ reference only.
Lack of diagnostic gold standard, children need to be vigilant when they have fever!
In the past month, six children with Kawasaki disease were treated in the pediatric department of a hospital in Xi ‘an, four of them were in serious condition, and one child also developed Kawasaki disease shock syndrome. What exactly is this disease? What’s the performance? Many parents said that they have never heard of it and have never seen it.
Let’s get to know Kawasaki disease through a case.
A boy, 1 year old and 5 months old, was admitted to the hospital because of "fever for 6 days".
Six days ago, the child had no obvious cause of fever, with a heat peak of 39.7℃, accompanied by runny nose, nasal obstruction, cough, shortness of breath, wheezing, convulsions, vomiting and diarrhea. Fever did not improve after 4 days of oral administration of cefaclor dry suspension in outpatient department.
Physical examination: conscious, ruddy complexion, palpable swollen lymph nodes on both sides of the neck, about 2cm*1cm in size, no tenderness, no redness and swelling, but movable, scattered red rash on the trunk skin, fading after pressure, conjunctival congestion, no purulent secretion, dry red lips, no chapped lips, red bayberry tongue, pharyngeal congestion, swollen tonsils on both sides, no purulent secretion. Flushing and swelling can be seen in the palm and sole, and no peeling is found at the toe end. Scar without redness, perianal flushing, peeling.
The child has no history of drug or food allergy, and is vaccinated on time.
Auxiliary examination: blood routine: white blood cell 17.06×109/L, neutrophil 72%, hemoglobin 105g/L, platelet 310×109/L, C-reactive protein 57 mg/L; ESR 80 mm/h; There is no abnormality in liver function; Anti-streptolysin O, seven respiratory virus antigens, mycoplasma pneumoniae PCR(-), normal immunoglobulin, blood culture (-); The right coronary artery diameter was 1.9mm and the left coronary artery diameter was 2.0mm by echocardiography.
Diagnosis: Kawasaki disease.
What is Kawasaki disease?
Kawasaki disease, also known as cutaneous mucosal lymph node syndrome, can’t be prevented, and the cause is still unclear. It is generally believed that Kawasaki disease is an acute systemic immune vasculitis triggered by infectious factors, with fever, jealousy, lip redness, rash and cervical lymph node enlargement as the main clinical manifestations. Cardiovascular injury, especially coronary artery disease, is an important complication of Kawasaki disease, which can lead to myocardial ischemia, myocardial infarction and even death, seriously endangering the health and life of children. Kawasaki disease mainly occurs in children under 5 years old, and can occur all year round, especially in East Asia such as China and Japan. The data published in recent years show that there are more than 100 new cases of Kawasaki disease per 100,000 children aged 0-4 every year.
What are the manifestations of Kawasaki disease?
Main clinical manifestations
1. Fever: It is often repeated fever, and the heat peak can reach 39-40℃, and antibiotic treatment is ineffective.
2. Changes of extremities: In the acute stage, the palms and soles flush and hard edema appear. At 2-3 weeks, desquamation (membranous desquamation) of fingers and toes starts from the nail week and can extend to the palms and soles of feet. The course of the disease lasts for 1-2 months, and deep transverse groove (Beau’s line) or nail removal may appear on the nail.

Fig. 1 Hard edema of palm (from UpToDate)

Fig. 2 membranous desquamation of hands and feet (from UpToDate)
3. Rash or redness at the BCG vaccination site: Rash usually appears within 5 days after fever, and there are common diffuse maculopapular rash, scarlet fever-like rash and erythema multiforme-like rash. Rash is usually widely distributed, mainly involving trunk and limbs. The aggravation of rash in groin and early desquamation, perianal flushing and desquamation are the characteristics of Kawasaki disease. Scar swelling is a relatively specific early manifestation of Kawasaki disease.

Figure 3 Rash of Kawasaki disease (from 2017 American Heart Association guidelines)

Fig. 4 Scar is red and swollen (I shot it myself).
4. Bilateral bulbar conjunctival congestion: Children may have bilateral bulbar conjunctival non-exudative congestion shortly after fever.

Fig. 5 bulbar conjunctival congestion (from UpToDate)
5. Oral and oral changes: including red lips, dryness, chapped lips, peeling and bleeding, strawberry tongue, and diffuse congestion of oropharyngeal mucosa.

Fig. 6 Dry red and chapped lips (from 2017 American Heart Association guidelines)

Figure 7 strawberry tongue (from UpToDate)
6. Non-suppurative enlargement of cervical lymph nodes: usually unilateral, with a diameter ≥1.5cm.
Auxiliary inspection
1. Laboratory inspection:
① Blood routine showed an increase in white blood cell count, mainly neutrophils; Decreased hemoglobin; The increase of platelet count usually appears in the second week of the course of disease, reaches its peak in the third week, and returns to normal in 4-6 weeks; A small number of children can have a decrease in platelet count, which indicates that the condition is serious.
② Urine routine showed leukocytosis, but urine culture was negative.
③C-reactive protein and serum amyloid A(SAA) increased, and erythrocyte sedimentation rate (ESR) increased.
④ Transaminase increased, total bilirubin increased, creatine muscle enzyme and myocardial isoenzyme increased, albumin and blood sodium decreased.
⑤ Serum inflammatory factors such as interleukin (IL)-6, IL-1 and tumor necrosis factor α (TNF α) are increased.
⑥ Plasma brain natriuretic peptide (BNP) or N-terminal pro-brain natriuretic peptide (NT?proBNP) increased, procalcitonin increased slightly and moderately, and serum ferritin and plasma dimer increased.
2. Echocardiography: Echocardiography should be performed as early as possible in the clinical diagnosis of Kawasaki disease to find out whether there is coronary artery damage, such as coronary artery dilatation or coronary artery aneurysm formation, and whether there is thrombosis should be paid attention to.
How to diagnose Kawasaki disease?
Kawasaki disease is a clinical syndrome, the diagnosis mainly depends on clinical manifestations, combined with laboratory examination and exclusion of other diseases. Kawasaki disease includes complete Kawasaki disease (CKD) and incomplete Kawasaki disease (IKD).
1.CKD: fever with at least 4 main clinical features of the following 5 items:
(1) bilateral bulbar conjunctival congestion;
(2) Oral and oral changes: dry and red lips, strawberry tongue and diffuse congestion of oropharynx mucosa;
(3) Rash, including red and swollen scar;
(4) Changes of extremities: redness and swelling of hands and feet in acute stage, and desquamation around nails in recovery stage;
(5) Non-suppurative cervical lymphadenopathy.
2.IKD: Children with fever ≥5d but with less than 4 main clinical features are assessed as IKD according to the flow chart in Figure 7.
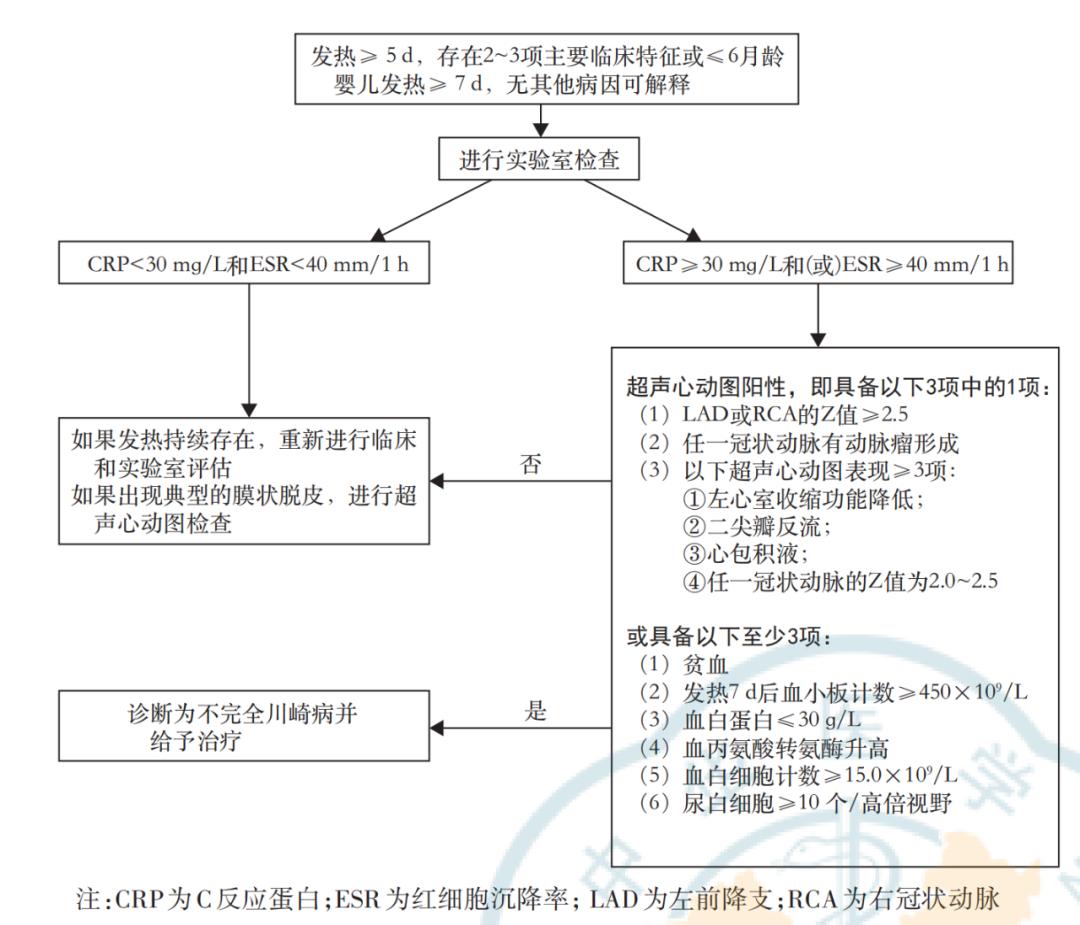
Fig. 8 Diagnostic flow chart of incomplete Kawasaki disease [1]
What conditions need to be considered for Kawasaki disease?
According to the 2017 American Heart Association guidelines, Kawasaki disease should be considered in the following situations:
(1) long-term fever and irritability of infants younger than 6 months;
② Infants have long-term fever and unexplained aseptic meningitis;
③ unexplained long-term fever or shock with negative blood culture in infants or children;
④ Infants or children have long-term fever and cervical lymphadenitis, and have no response to antibiotic treatment;
⑤ Infants or children have long-term fever, retropharyngeal or parapharyngeal cellulitis, and have no response to antibiotic treatment.
Kawasaki disease needs to be differentiated from which diseases.
1. Scarlet fever: Kawasaki disease can also have a scarlet fever-like rash, but the simple scarlet fever infection is mostly effective for antibiotic treatment. After antibiotic treatment, the symptoms are improved and the inflammatory index is obviously reduced.
2. Other virus infections (such as adenovirus, enterovirus): In virus-infected blood, the routine white blood cell count is not high or low, but lymphocytes are increased, C-reactive protein, SAA and ESR are often not significantly increased, and the virus antibody in blood can be significantly increased.
3. Septic shock syndrome caused by staphylococci and streptococcal toxins: It needs to be differentiated from Kawasaki disease shock syndrome, especially when antibiotic treatment is ineffective, closely observe the other five characteristic clinical manifestations of Kawasaki disease except fever, and conduct echocardiography in time.
4. Drug hypersensitivity such as Stevens Johnson syndrome: There is a history of using sensitive drugs, and the mucosal manifestations are usually more serious. Moreover, the ocular symptoms are not only conjunctival congestion, but also catarrhal, suppurative and pseudomembranous conjunctivitis, which can leave eye complications.
How to treat Kawasaki disease?
Although Kawasaki disease cannot be prevented, it can be treated. Once it is diagnosed, it should be treated as soon as possible:
① High-dose intravenous immunoglobulin (IVIG): 2g/kg, the infusion time is usually 10-12h, and the dosage of 1g/kg per day can be used for children with heavy weight (such as > 20kg) for two days.
② Anti-inflammatory effect of aspirin: 30-50mg/(kg d), taken orally for three times. If the diagnosis of Kawasaki disease is delayed for more than 10 days or even longer, it is still recommended to give the above treatment as long as there are clinical symptoms and/or inflammatory indicators are still abnormal; If the clinical symptoms have subsided, the inflammatory indicators have returned to normal, and echocardiography shows no coronary artery lesions, only subsequent antiplatelet therapy and follow-up can be given.
③ Anti-platelet effect of aspirin: After 48-72h, the inflammatory indexes (white blood cell count and C-reactive protein) returned to normal, and aspirin was reduced to 3-5mg/kg. For children with no coronary artery disease or mild coronary artery dilatation in acute phase but returning to normal within 30 days, aspirin will continue to be used for 2-3 months.
Difficulties in diagnosis and treatment of Kawasaki disease in children
1. Kawasaki disease mainly depends on the clinical features, combined with the manifestations of systemic multi-system vasculitis and laboratory examination for clinical diagnosis, which lacks the gold standard and needs to exclude other diseases. The diagnosis of CKD is usually not difficult, but for the diagnosis of IKD and severe Kawasaki disease, clinicians need to be highly vigilant, combine laboratory indicators with echocardiography to make a comprehensive judgment, and sometimes even need dynamic observation during the course of the disease to make a diagnosis.
2. The main clinical features of Kawasaki disease rarely appear at a single point in time, and some clinical features will fade within a few days, so it is necessary to ask the medical history and physical examination carefully. Kawasaki disease is a self-limited disease, and the fever can stop automatically. Clinicians may ignore the main clinical manifestations of Kawasaki disease because of the cessation of fever, thus delaying the diagnosis and failing to improve echocardiography in time to evaluate whether there is coronary artery damage.
3. Kawasaki disease is systemic vasculitis, with multiple system injuries. The first symptom can be some specific organ injuries, and sometimes it is misdiagnosed as other diseases, such as urinary tract infection, suppurative lymphadenitis or mumps, acute abdomen, hepatitis and arthritis.
Summary:
Simple fever in the early stage of Kawasaki disease may be mistaken for a cold. Parents should see a doctor again in time for children with repeated fever with rash, jealousy and red lips. For children with fever for more than 5 days and poor antibiotic treatment effect, clinicians should consider the possibility of Kawasaki disease, ask for medical history and physical examination in detail, dynamically follow up relevant auxiliary examinations, and improve echocardiography in time. Children treated with IVIG rarely die of Kawasaki disease, and most of them have a good prognosis. The long-term complications are mainly related to the degree of coronary artery involvement. Take medicine according to the doctor’s advice after discharge, follow up regularly for fever and review echocardiography to evaluate the heart involvement.
References:
[1] Cardiology Group of Pediatrics Branch of Chinese Medical Association, Rheumatology Group of Pediatrics Branch of Chinese Medical Association, Immunology Group of Pediatrics Branch of Chinese Medical Association, etc. Expert Consensus on Diagnosis and Acute Treatment of Kawasaki Disease [J]. Chinese Journal of Pediatrics, 2022,60 (1): 613.
[2]McCrindle BW, Rowley AH, Newburger JW, et al. Diagnosis, treatment, and long?term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association[J]. Circulation, 2017, 135(17): e927?e999.
[3]Fukazawa R, Kobayashi J, Ayusawa M, et al. JCS/JSCS 2020 guideline on diagnosis and management of cardiovascular sequelae in Kawasaki disease[J]. Circ J, 2020, 84(8):1348?1407.
The wonderful case you want to see
There are "pediatric cases" columns in the doctor’s station.
1. Scan the QR code below
2. Click "Download Now"


3. Open the doctor station App and click on the column.

4. Find "pediatric cases" in case sharing.
Focus on the column


Subscribe to the column and read a good case every day!
Download the doctor station App and subscribe anytime, anywhere ~
This article is the first: Pediatric Channel of Medical Science
Author: PerrineWANG
Editor in charge: Wen
Recommended reading
Copyright statement
This article is original, welcome to forward the circle of friends.
– End –
Read the original text